Do You Have Leaky Gut Syndrome?
What is leaky gut syndrome? How does it impact your health? Continue reading to get the answer.
Food enters the mouth and moves through the Digestive System, leaving via the anus. Much of it never really enters the body. Think of water entering a tube and exiting the other end. Your digestive tract has a protective barrier that keeps harmful bacteria, toxins, and undigested food separate from the bloodstream, where it can damage your body. When gaps develop between the cells lining the gut, leaky gut syndrome develops. A staggering 80-90% of Americans are affected by leaky gut syndrome today. To make matters worse, each of your 7 Systems can be harmed when this protective barrier is compromised.
Rhonda was one of those who had this syndrome. It led to her developing irritable bowel syndrome (IBS) symptoms and many other health problems.
Rhonda did not need to lose much weight but joined the 7 Systems Plan to resolve her affliction with (IBS). For years, she had to plan her outings around the availability of a bathroom. She was annoyed that she couldn’t go out with her girlfriends.
Ninety days after starting the 7 Systems Plan, her IBS was gone, she was at her ideal weight, and her Digestive System was working correctly. She once again could enjoy going out whenever she wanted.
Let’s delve into the detrimental effects of a leaky gut on your overall health and how to heal the gut.
Key Questions to Evaluate Gut Health:
What foods are you taking in? Are you reactive to them? Are you chewing?
How’s your digestion relative to stomach acids, gallbladder, and pancreas function?
Is stress a factor?
What type of bugs live in your gut?
How often do you have a bowel movement and what is the transit time?
Do you have a leaky gut?
Do symptoms worsen with probiotic supplementation?
Is there small intestine bacterial overgrowth (SIBO), often associated with inflammatory bowel disorders)?
Leaky Gut
Leaky gut is a common factor contributing to gastrointestinal issues in individuals with chronic illnesses. Many patients experienced conditions like colic or recurrent ear infections during early life, exposing them to antibiotics. Antibiotics disrupt the balance of microorganisms in the gut, leading to dysbiosis, which can cause a leaky gut.
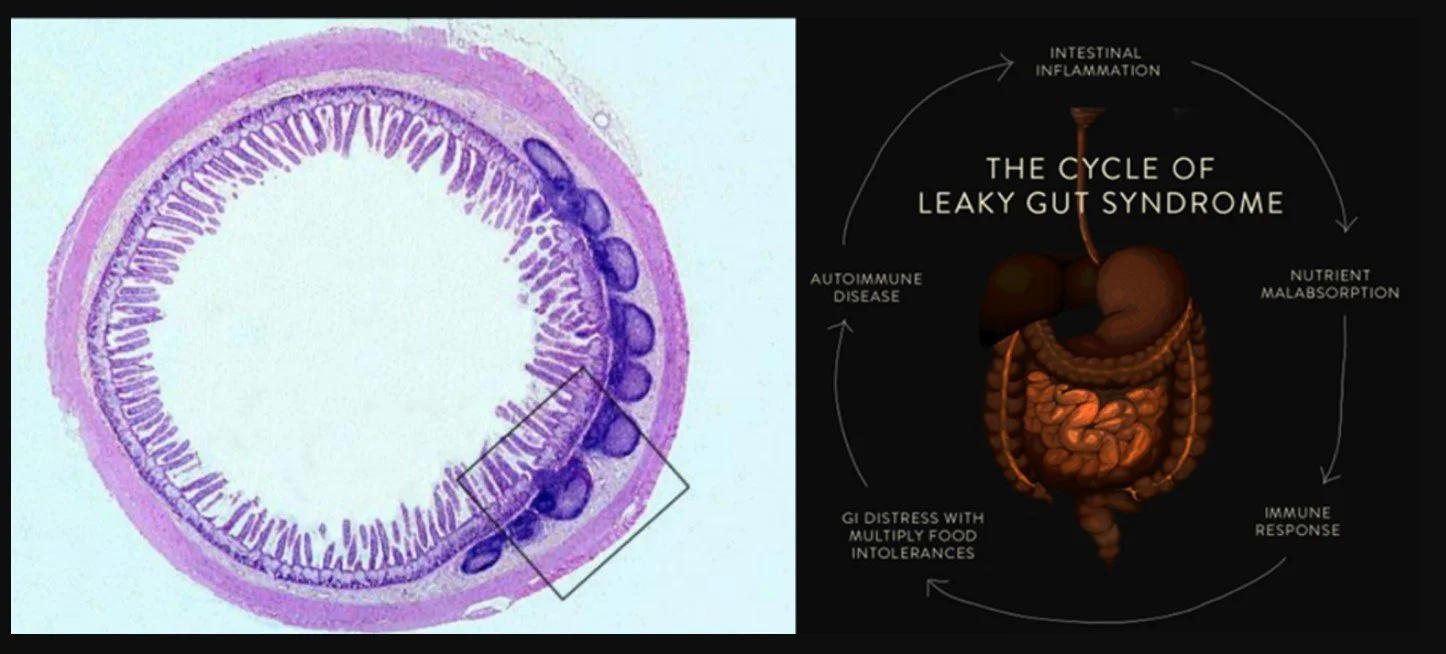
Gastrointestinal function extends beyond digestion and nutrient absorption. The gut is home to a diverse microbiome. Dysbiosis occurs when this microbiome becomes imbalanced, resulting in inflammation. This inflammation can cause the mucous membranes to become permeable, allowing microorganisms and food particles to interact abnormally with the immune system. Consequently, the body perceives partially digested food particles as invaders, triggering the immune system to produce antibodies against them. This immune response leads to the development of food sensitivities and allergies.
The Cause of Leaky Gut
If you suspect you have leaky gut syndrome, you can take steps to address its root cause. External factors such as food, infections, toxins, and stress should be eliminated or minimized, and a healthy diet, probiotics, and functional foods such as Dynamic GI Restore can help to heal the gut and restore your health. A properly functioning Digestive System is critical to good health, and repairing a leaky gut can positively impact many chronic health problems. So, take care of your gut, and your body will thank you.
Leaky gut syndrome can arise from various factors, with poor dietary choices being one of the primary culprits. Processed foods containing gluten are significant, as they have ingredients that can lead to the breakdown of tight junctions in the intestinal lining. Other inflammatory or toxic foods, such as dairy, sugar, and alcohol, can also contribute to this issue. Beyond dietary factors, infections, unfriendly microbes, toxins, and stress can also trigger leaky gut symptoms.
Infections caused by Candida (yeast) overgrowth, intestinal parasites, and SIBO are among the most common causes of leaky gut. Toxins, which can come from medications such as NSAIDs, steroids, antibiotics, and acid-reducing drugs, can also significantly impact digestion. Environmental toxins like mercury, pesticides, and BPA found in plastics are other potential causal agents.
Stress is another factor that can cause leaky gut syndrome. When the body is under stress, it releases hormones that affect the Digestive System and cause inflammation, leading to a potential breakdown in the gut lining.
Effects on the Brain
Leaky gut doesn’t solely impact the body’s relationship with food; it can also trigger chronic inflammation, activating microglia, the white blood cells of the brain, and producing antibodies against specific parts of the brain. Leaky gut can also compromise the protective blood-brain barrier, allowing substances that shouldn’t enter the brain to do so.
Your Defense System and Inflammation
The gut houses around 80% of the body’s immune cells and boasts an intestinal surface area approximately the size of a football field. The immune system in the gut, known as gut-associated lymphoid tissue or GLT, safeguards the body against germs in food.
Gut lymph tissue surrounding intestines.
Inflammation within the gut facilitates the passage of bacteria, bacterial fragments, intact or partially intact proteins, and other pathogens into the body’s circulation. This contributes to systemic inflammation and also impairs nutrient absorption.
Intestinal barrier breakdown can occur due to intestinal infections or stress. In a normal response, immune system components work together to heal the injury and control invading bacteria. However, when this response is faulty and a leaky barrier emerges, the risk of developing inflammatory bowel disease (IBD) increases.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is an umbrella term encompassing chronic digestive tract inflammation disorders. This group of disorders primarily affects the intestines, causing redness and swelling.
The following conditions fall under the category of inflammatory bowel disease (IBD):
Crohn’s Disease: Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus. It commonly causes inflammation in the small intestine and the beginning of the large intestine (colon). Inflammation can occur in patches and affect intestinal wall thickness.
Ulcerative Colitis: Unlike Crohn’s disease, which can affect any part of the digestive tract, ulcerative colitis is limited to the colon and rectum. It causes continuous inflammation and ulcers in the innermost lining of the colon.
Crohn’s disease and ulcerative colitis share similar symptoms, such as abdominal pain, diarrhea, rectal bleeding, fatigue, and weight loss. However, there are differences in inflammation patterns and the specific symptoms individuals with these conditions experience.
Study Links Common Food Additives to Crohn’s Disease: Common additives in ice cream, margarine, packaged bread, and many processed foods may promote inflammatory bowel diseases, ulcerative colitis, Crohn’s disease, and metabolic syndrome.
Migraine Linked to Irritable Bowel Syndrome: Called the Brain-Gut Axis, migraine and tension-type headaches may share links with irritable bowel syndrome (IBS). Test results suggest a high possibility of phenotypic and genotypic associations between IBS and primary headache disorders (particularly migraine) and support the presence of some shared pathophysiology.
Celiac disease: This immune system disorder causes a heightened sensitivity to gluten, a protein found in wheat, rye, and barley. When someone with celiac disease consumes gluten, their immune system mistakenly attacks its own body tissues and organs. This can lead to many symptoms throughout the body if a strict, lifelong gluten-free diet is not followed.
Recent research suggests that celiac disease is more common than previously thought. A large study revealed that nearly two million people in the United States have celiac disease, but most are unaware. The condition can develop at any age after starting to eat gluten-containing foods.
The main symptoms of celiac disease stem from inflammation in the gastrointestinal tract which damages the tiny finger-like projections called villi in the small intestine responsible for absorbing nutrients. As a result, people with celiac disease may experience diarrhea, weight loss, abdominal pain, swelling, and food intolerances. Additionally, celiac disease is linked to an increased risk of certain gastrointestinal cancers affecting the small intestine and esophagus.
Managing celiac disease involves adhering to a gluten-free diet to prevent inflammation and its associated symptoms. By avoiding gluten, individuals with celiac disease can improve their overall well-being and maintain a healthier life.
The Function of Beneficial Microbiome:
The beneficial microbiome digests food and produces enzymes that metabolize protein into absorbable amino acids. These essential enzymes also transport vital vitamins, minerals, and other nutrients through the intestinal wall and into the bloodstream, where they are effectively carried to cells that need these nutrient packages.
These beneficial species also help the body produce and metabolize vitamins K2, B1, B2, B3, B6, B12, folate & pantothenic acid. Without adequate microbiome production, the body will suffer from poor calcium metabolism, neuromuscular function, and chronic inflammatory conditions due to deficiencies in these crucial nutrients.
Gut membrane healing is a 5-step process:
1) Remove toxins, inflammatory foods, and harmful microbes.
2) Replace missing enzymes and acids and add healing foods.
3) Repair the mucosal membrane and leaky gut.
4) Reinoculate with beneficial microbes.
5) Retain your new healthy gut.
Many individuals fail to repair their gut membrane. My go-to supplement for the repair process is Dynamic GI Restore. Nutrients and herbs help heal and seal the gut membrane and replenish the mucosal membrane. This has been a core product for individuals trying to improve their gut function, reverse autoimmunity, reduce pain, and restore function. We will explore the 5-R program in future newsletters.
Avoid Antibiotics:
Antibiotics are the most lethal thing for our microbial balance. After a round of antibiotics, re-establishing gut balance will take at least four to eight weeks. This period is an opportunistic window for parasites to make themselves homes on the gut wall. Eating conventional meat, dairy, and poultry products can be as dangerous as taking antibiotic prescriptions due to the amount of antibiotics present.
Medications of all types, including contraception pills and corticosteroids, are highly hazardous to the gut microbiome. Chlorinated water is particularly dangerous as it sterilizes our gut, and repeated exposure destroys the good bacteria. Dental fluoride treatments and fluoride-based toothpaste damage the microbial balance. However, practice good dental hygiene because neglecting dental health can lead to infection and inflammation.
Use Probiotics:
A diet high in fermented foods and essential fats and low in sugar and other toxic food sources will increase the number of beneficial microbes. Probiotic supplements are necessary to speed up the re-inoculation time as well. UltraBiotic Daily Strain is my favorite probiotic.
Video of the Week:
Recipe of the Week:
From Teresa’s 7 Systems Kitchen
Avoid gluten and try this idea:
Banza Spaghetti (made from Chickpeas) from Thrive Market.
Follow pkg directions using filtered water.
Grass fed beef. Browned in a stainless steel or cast-iron skillet.
Thrive Market organic tomato sauce in a jar (choose your favorite flavor).
Combine ingredients and serve with side salad with healthy dressing or vinegar and oil.